Osteoporosis and Type 2 Diabetes
Despite evidence for higher fracture risk, clinical effects of osteoporosis treatments in type 2 diabetes (T2D) are largely unknown. Post hoc analyses (A post hoc test is used whenever a significant difference between three or more sample means has been revealed) of the DANCE observational study compared T2D patients and patients without diabetes to assess the effect of teriparatide. An osteoanabolic therapy on skeletal outcomes and safety.
Patients included ambulatory men and women with osteoporosis receiving teriparatide 20 μg/day SQ up to 24 months followed by observation up to 24 months. Main outcome measures included nonvertebral fracture incidence comparing 0–6 months with 6+ months of teriparatide. Change from baseline in BMD and back pain severity, and serious adverse events. Analyses included 4042 patients; 291 with T2D, 3751 without diabetes.
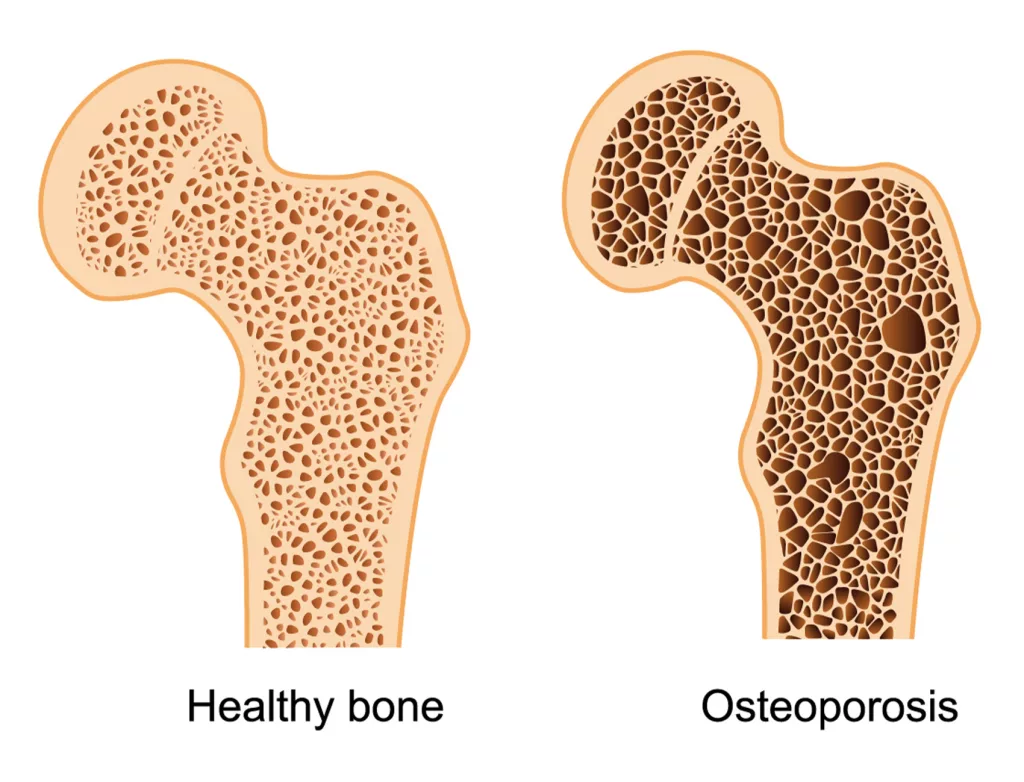
Osteoporosis ICD 10: Understanding Treatment Outcomes in T2D and Non-Diabetic Patients
Osteoporosis, a common condition characterized by reduced bone density, often leads to fractures, posing significant health challenges. In clinical settings, accurate documentation using codes like osteoporosis ICD 10 (M81.0 for age-related osteoporosis without current pathological fracture) is crucial for diagnosis and management. This article examines the effects of teriparatide treatment on fracture incidence and bone mineral density (BMD) in patients with and without type 2 diabetes (T2D).
Fracture Incidence: T2D vs. Non-Diabetic Patients
The fracture incidence for T2D patients was 3.5 per 100 patient-years during the initial 0–6 months of treatment and decreased to 1.6 per 100 patient-years from 6 months to treatment end—a 47% reduction from baseline (95% CI 12–187%). For non-diabetic patients, the fracture incidence was slightly lower at 3.2 during the first 6 months, dropping to 1.8 during subsequent treatment (57% of baseline, 95% CI 39–83%). These findings indicate a significant reduction in nonvertebral fractures across both groups during teriparatide treatment.
Key Determinants of Fracture Outcome
Analysis revealed that:
- Diabetes Status: Diabetes was not a significant determinant of fracture outcomes (P = 0.858).
- Treatment Duration: Duration played a significant role in reducing fracture risk (P = 0.003).
- Group Comparisons: The effect of treatment duration did not differ significantly between T2D and non-diabetic groups (interaction P = 0.792)
Bone Mineral Density (BMD) Improvements
Increases in BMD were a key outcome of teriparatide treatment:
- Spine and Total Hip BMD: Improvements were similar for both groups.
- Femoral Neck BMD: T2D patients experienced a greater increase (+0.34 g/cm²) compared to non-diabetic patients (+0.004 g/cm²; P = 0.014).
- These results highlight the efficacy of teriparatide in improving BMD, particularly in the femoral neck, for T2D patients.
Decrease in Back Pain Severity
Both groups reported a significant reduction in back pain severity, adding to the overall benefits of the treatment.
Safety and Tolerability
Teriparatide was well tolerated in both T2D and non-diabetic groups, with no new safety concerns identified during the study.
Conclusion
Teriparatide treatment led to a significant reduction in nonvertebral fracture incidence, an increase in BMD, and decreased back pain severity, with similar outcomes for T2D and non-diabetic patients. For healthcare providers managing osteoporosis, documenting the condition using appropriate osteoporosis ICD 10 codes ensures comprehensive patient care and better monitoring of treatment outcomes.
References
http://www.healio.com/endocrinology/diabetes/news/in-the-journals/%7B9f3f2586-dcdb-4b07-bdb0-b822e302b26b%7D/more-sensitive-medication-adherence-measures-needed-for-high-risk-diabetes