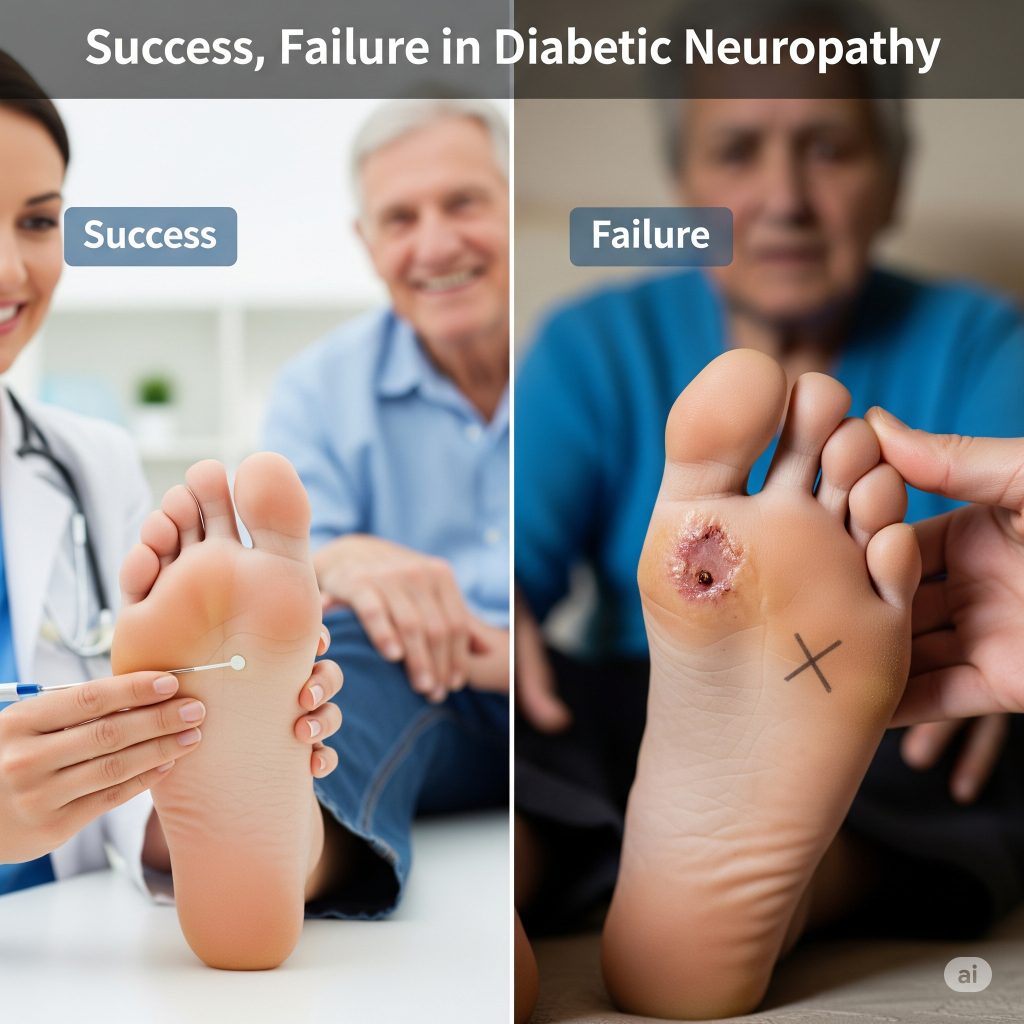
Success, Failure in Diabetic Neuropathy – The American Diabetes Association’s (ADA) most recent guidelines revise neuropathy recommendations last published in 2004. The document, published in Diabetes Care, addresses prevention and management of distal symmetric polyneuropathy*, diabetic autonomic neuropathies, including cardiovascular autonomic neuropathy**, and other forms of neuropathy.
According to the authors, electrophysiologic testing or referral to a neurologist is rarely needed to diagnose neuropathy. For treating neuropathic pain, the report advises pregabalin or duloxetine as first-line treatments. Opioids are advised only for patients with severe pain who have not responded to other treatment options. The document does not give any recommendation for disease-modifying treatments, as none are approved by the U.S. Food and Drug Administration.
* Polyneuropathy = damage or disease affecting peripheral nerves (peripheral neuropathy) in roughly the same areas on both sides of the body, featuring weakness, numbness, and burning pain.
** Autonomic Neuropathies = a group of symptoms that occur when there is damage to the nerves that manage every day body functions such as blood pressure, heart rate, sweating, bowel and bladder emptying, and digestion.
New ADA Guidance Charts Success, Failure in Diabetic Neuropathy
Notably missing from the first US guidelines to address diabetic neuropathy in more than a decade is any recommendation for disease-modifying treatments, since none are currently approved by the US Food and Drug Administration (FDA).
Indeed, many candidate drugs for diabetic neuropathy have failed in trials, and one of the new guideline authors believes novel end points — particularly measures of small-nerve fiber damage and repair — that could better assess a potential drug’s efficacy need to be employed in clinical studies.
Coauthor Rayaz A Malik, MBChB, FRCP, PhD, of Weill Cornell Medicine-Qatar, Doha and New York, told Medscape Medical News, “As a clinician, I’m frustrated that current drugs have no benefit for the underlying nerve damage. We have witnessed failure after failure of clinical trials of disease-modifying drugs, because the end points are not fit for that purpose.”
Assessment for Earlier Diagnosis of Diabetic Neuropathy
Such assessments of small-nerve fiber damage should also be used for earlier diagnosis of diabetic neuropathy, says Dr Malik.
“Although about 20% of patients have painful neuropathy and can present to their doctor, the majority have painless neuropathy, which is silent and is diagnosed only when it is too late and the patient has already developed a foot ulcer,” he continued.
5-year Mortality Rate for Foot Ulcer Patients
“Given that the 5-year mortality of a patient with a foot ulcer is worse than most cancers, there is a need to identify early neuropathy. Yet currently advocated tests, like the monofilament, identify only patients with advanced neuropathy. Why do we have robust methods for detecting early retinopathy (diseased retina, the nerve of the eye) and nephropathy (kidney disease), but not neuropathy?”
Published in the January issue of Diabetes Care, the new ADA position statement revises ADA’s last neuropathy guideline, published in 2004.
The new document covers prevention and management of distal symmetric polyneuropathy (DSPN), diabetic autonomic neuropathies including cardiovascular autonomic neuropathy (CAN), as well as less common forms of neuropathy.
The aim is to provide state-of-the-art information for clinical management of the condition but to also acknowledge the current lack of disease-modifying drugs.
http://www.medscape.com/viewarticle/874162#vp_1