Speeding Health Devices to Market
The FDA’s Expedited Access Pathway (EAP) program, launched in April 2015, is designed to help speed innovative and life-saving Health devices to market.
Speeding Health Devices to Market – FDA’s Expedited Access Pathway (EAP) Program – A year-old FDA program designed to help innovative m Health companies speed their potentially life-saving products to market has so far accepted more than half of its applicants.
In all, 17 of 29 applications for the U.S. Food and Drug Administration’s Expedited Access Pathway (EAP) program, launched last April 15 by the FDA’s Center for Devices and Radiological Health, have been approved.
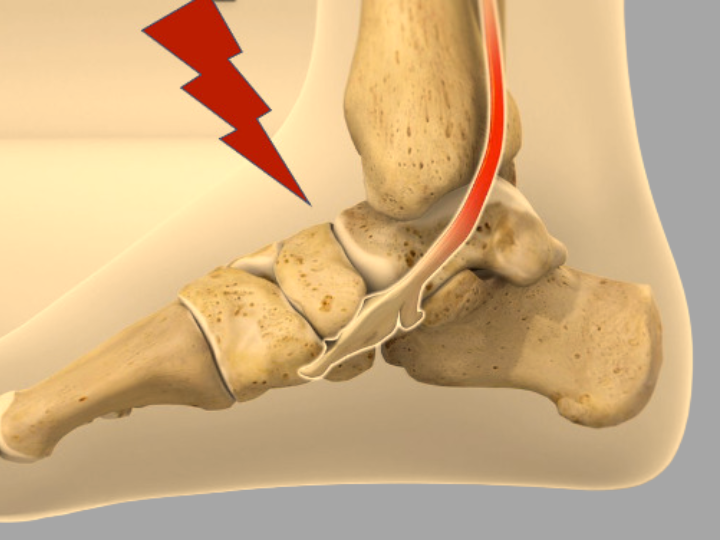
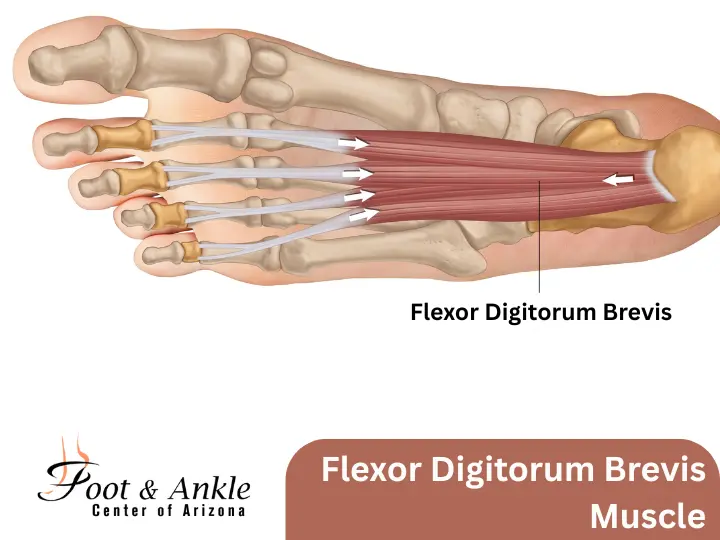
The EAP program is designed for devices that address the toughest conditions and would file a Pre-Market Approval (PMA) application or de novo request (de novo means “new trial:). A device would qualify for the program if no other reliable therapeutic or diagnostic options are available, or the device must be a “breakthrough technology,” have important advantages over any alternatives or be in the best interest of patients. To qualify for the program, an applicant must meet three conditions:
- The device should treat or diagnose a life-threatening or “irreversibly debilitating” disease or condition;
- The device should address an unmet need; and
- The company should have a data development plan outlining what will be included in future submissions to the FDA.
FDA officials Jeffrey Shuren, MD, JD, director of Center for Devices and Radiological Health; Erin Cutts, BS, policy lead for the Q-Submission Program (acting) in the center’s Office of Device Evaluation; and Owen Faris, PhD, clinical trials director in the center’s Office of Device Evaluation, offered up the statistics in a recent blog on the program’s one-year anniversary.
“EAP designation requests have included devices for the heart, brain, and kidneys that are manufactured by small start-up companies and large corporations,” they wrote. “We expect that our resources and focus on these promising technologies under the EAP program will allow them to be evaluated and enter the market more quickly, therefore providing options to the patients who need them most.”
Program Inclusion Conditions per Regulatory Affairs Professionals Society:
- Premarket (clinical or non-clinical) data demonstrate that the probability of serious harm is low;
- Post market patient exposure to the device prior to the required submission of post market data to FDA will be small;
- The EAP program is designed for devices that address the toughest conditions and would file a PMA application or de novo request.
A device would qualify for the program if no other reliable therapeutic or diagnostic options are available, or the device must be a “breakthrough technology,” have important advantages over any alternatives or be in the best interest of patients. To qualify for the program, an applicant must meet three conditions:
-
- The device should treat or diagnose a life-threatening or “irreversibly debilitating” disease or condition;
- The device should address an unmet need; and
- The company should have a data development plan outlining what will be included in future submissions to the FDA.
http://mhealthintelligence.com/news/fdas-mhealth-innovation-program-sees-success-in-its-first-year